fix your eyes
on what matters most
Myopia (Nearsighted) Treatment in Melbourne & Brevard County, FL
Do you struggle reading road signs and discerning faces until you’re nearly passing them? You could be suffering from myopia, otherwise known as nearsightedness. Luckily, you have a wide variety of treatment options at your disposal.
HOW DO I KNOW IF I HAVE MYOPIA?
Symptoms
If you have myopia, you may see signs of the following:

Diagnosis/ Testing for Myopia
Our first-in-class technology suite provides better detection & better outcomes for your vision health.
-
Eye Health Assessment
-
Muscle Function Test
-
Visual Acuity or Refraction Test
-
Binocular Vision Skills Assessment
-
Eye Pressure Test
-
Color Vision Screening
Eye Health Assessment
This assessment uses an ophthalmoscope to examine different parts of your eye. This is a handheld piece of equipment that the doctor will use to examine your eyes with a light adjusted to the right aperture and filter necessary to see to the back of your eye.
Why We Use This Method:
- This tool allows the doctor to evaluate your pupil responses, optic nerve, retina, cornea, and lens.
- We use this tool to look for signs of eye diseases or retinal vascular diseases
Muscle Function Test
If you’ve ever had an optometrist ask you to follow an object with only your eyes without moving your head then you’ve completed a muscle function test. The object, commonly a pen or pencil, will be held 40cm from your face while the assessment is completed and generally takes less than 30 seconds to complete. This is performed to check the movement of your eyes in each direction and at specific angles. The doctor will then be able to determine muscle weakness or involuntary eye movement.
Why We Use This Method:
- This checks for uncontrolled eye movement or double vision in patients.
- We’re also able to identify the following potential problem: nystagmus, strabismus, mechanical restrictions due to traumatic injury.
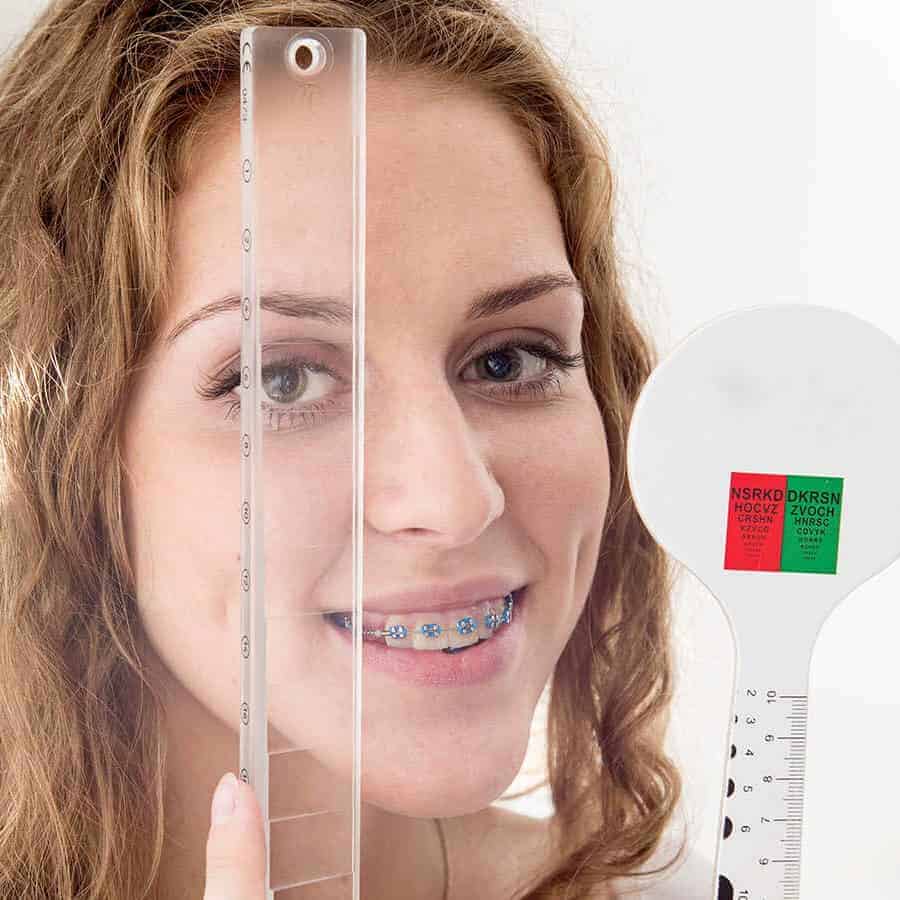
Visual Acuity or Refraction Test
Visual acuity, otherwise known as a refraction test, is used to determine the degree to which you may be nearsighted, farsighted or have astigmatism. It is performed via computerized test, machine, or by hand. The doctor is looking at the amount of light reflected by your retina to determine your refractive score. This refractive score is one half of your eyeglass or contact prescription.
The second part of your prescription is determined using a Phoroptor. It seems complicated and scary, but most people are familiar with this particular piece of equipment. This is pushed in front of your eyes and used as a mask for you to look through. At this point, you will read a chart of letters located roughly 20 feet from where you’re seated.
Why We Use This Method:
- With refractive tests we can identify the following refractive errors: astigmatism, presbyopia, myopia, and hyperopia.
- With this test we can diagnose macular degernations, retinal vessel occlusion, retinitis pigmentosa, and retinal detachment.
Binocular Vision Skills Assessment
Binocular vision skills assessment aren’t routinely performed on every patient. But if patients complain of indicative symptoms this can be completed to make sure they aren’t suffering from a difficult to detect visual deficit. Failing this assessment could point to you suffering from improper depth perception, poor eye muscle coordination and the inability to change focus from near to far objects.
Why We Use This Method:
- If patients are suffering from the following symptoms we will conduct a binocular vision skills assessment: double vision, headaches, eyestrain, and patients with a traumatic brain injury.
- This assessment identifies the following: oculomotor dysfunctions, accomodative dysfunction, binocular vision dysfunction, strabismus, visual perceptual deficits.
Eye Pressure Test
Your doctor may administer one or more tests to evaluate your intra-ocular pressure. One commonly used test is through the use of a machine, that puffs air into your eye to test IOP call a non-contact tonometry (NCT). The eye bounces the air back to a sensor that reads the pressure automatically. While unpleasant, this test is not painful.
An alternative way to perform this test in the case of a NCT machine being unavailable is through manual testing. Eye drops will be administered and then gentle pressure will be applied to the surface of your eye by the ophthalmologist or using a blue light instrument. This will feel like placing a contact lense in your eye.
The desired range for eye pressure will vary from person to person but your ophthalmologist will determine the correct range for you individually. High intra-ocular pressure could point to glaucoma developing in your eyes which will need to be addressed further by the ophthalmologist.
Why We Use This Method:
- The major purpose behind testing eye pressure is to identify eyes developing glaucoma.
Color Vision Screening
Color vision screening is used to see how you perceive colors. Color blindness doesn’t generally affect everyday life. It is usually tested using a form of the Ishihara but more intensive forms of assessment are available. Extensive exams look into the type and severity of color blindness while color vision screening only shows if there is a color vision problem.
Why We Use This Method:
- Identifying color blindness, especially in children, can explain poor performance or learning frustrations.

Eye Health Assessment
This assessment uses an ophthalmoscope to examine different parts of your eye. This is a handheld piece of equipment that the doctor will use to examine your eyes with a light adjusted to the right aperture and filter necessary to see to the back of your eye.
Why We Use This Method:
- This tool allows the doctor to evaluate your pupil responses, optic nerve, retina, cornea, and lens.
- We use this tool to look for signs of eye diseases or retinal vascular diseases

Muscle Function Test
If you’ve ever had an optometrist ask you to follow an object with only your eyes without moving your head then you’ve completed a muscle function test. The object, commonly a pen or pencil, will be held 40cm from your face while the assessment is completed and generally takes less than 30 seconds to complete. This is performed to check the movement of your eyes in each direction and at specific angles. The doctor will then be able to determine muscle weakness or involuntary eye movement.
Why We Use This Method:
- This checks for uncontrolled eye movement or double vision in patients.
- We’re also able to identify the following potential problem: nystagmus, strabismus, mechanical restrictions due to traumatic injury.

Visual Acuity or Refraction Test
Visual acuity, otherwise known as a refraction test, is used to determine the degree to which you may be nearsighted, farsighted or have astigmatism. It is performed via computerized test, machine, or by hand. The doctor is looking at the amount of light reflected by your retina to determine your refractive score. This refractive score is one half of your eyeglass or contact prescription.
The second part of your prescription is determined using a Phoroptor. It seems complicated and scary, but most people are familiar with this particular piece of equipment. This is pushed in front of your eyes and used as a mask for you to look through. At this point, you will read a chart of letters located roughly 20 feet from where you’re seated.
Why We Use This Method:
- With refractive tests we can identify the following refractive errors: astigmatism, presbyopia, myopia, and hyperopia.
- With this test we can diagnose macular degernations, retinal vessel occlusion, retinitis pigmentosa, and retinal detachment.
Binocular Vision Skills Assessment
Binocular vision skills assessment aren’t routinely performed on every patient. But if patients complain of indicative symptoms this can be completed to make sure they aren’t suffering from a difficult to detect visual deficit. Failing this assessment could point to you suffering from improper depth perception, poor eye muscle coordination and the inability to change focus from near to far objects.
Why We Use This Method:
- If patients are suffering from the following symptoms we will conduct a binocular vision skills assessment: double vision, headaches, eyestrain, and patients with a traumatic brain injury.
- This assessment identifies the following: oculomotor dysfunctions, accomodative dysfunction, binocular vision dysfunction, strabismus, visual perceptual deficits.

Eye Pressure Test
Your doctor may administer one or more tests to evaluate your intra-ocular pressure. One commonly used test is through the use of a machine, that puffs air into your eye to test IOP call a non-contact tonometry (NCT). The eye bounces the air back to a sensor that reads the pressure automatically. While unpleasant, this test is not painful.
An alternative way to perform this test in the case of a NCT machine being unavailable is through manual testing. Eye drops will be administered and then gentle pressure will be applied to the surface of your eye by the ophthalmologist or using a blue light instrument. This will feel like placing a contact lense in your eye.
The desired range for eye pressure will vary from person to person but your ophthalmologist will determine the correct range for you individually. High intra-ocular pressure could point to glaucoma developing in your eyes which will need to be addressed further by the ophthalmologist.
Why We Use This Method:
- The major purpose behind testing eye pressure is to identify eyes developing glaucoma.
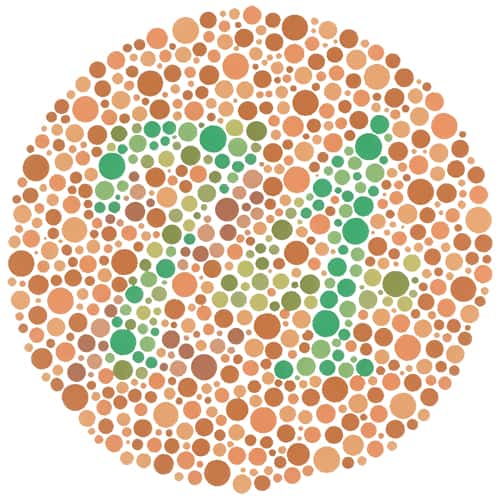
Color Vision Screening
Color vision screening is used to see how you perceive colors. Color blindness doesn’t generally affect everyday life. It is usually tested using a form of the Ishihara but more intensive forms of assessment are available. Extensive exams look into the type and severity of color blindness while color vision screening only shows if there is a color vision problem.
Why We Use This Method:
- Identifying color blindness, especially in children, can explain poor performance or learning frustrations.
START SEEING CLEARER
Treatment Options
Restore your vision & restore your life with the most modern myopia treatments available today.

FEATURED TREATMENT OPTION
LASIK
LASIK treatments offers a no-lens solution, permanent or otherwise, for your nearsightedness. Walk away from your procedure with improved vision and no stitches. Start living life with clearer vision when you choose LASIK vision correction.
Schedule A Consultation or learn more
Myopia FAQ
-
Who is at risk of developing myopia?
Children will usually begin to showing signs of myopia when they are between the ages of 8 and 12. This is when their eyes are growing and changing. Other indicating signs you can look out for include:
- Parents with myopia
- Consistent, close-up work
- Diabetes or other health concerns
-
What happens if myopia is left untreated?
If left untreated, your myopia could be a risk factor to develop more severe eye concerns such as cataracts, glaucoma, and retinal detachment.
-
How can I prevent myopia from worsening?
Practice the following techniques to keep myopia from worsening:
- Increase exposure to natural daylight
- Keep rooms well-lit when completing close-up work
- Don’t hold reading material or electronics too close to your eyes
-
What causes myopia?
We know what causes nearsightedness within the eye but not the exact cause for the refractive error to originally develop in specific eyes. However, the frequency you complete intensive visual work like reading or using a computer could contribute to your development of myopia.
-
Is myopia hereditary?
Research points to myopia being more commonly developed by those who have two parents also suffering from myopia. Having parents with myopia may not mean you will develop it as well, but it does suggest you will be more likely to develop myopia at some point in your life.
-
How can I prevent myopia in my eyes?
Increased exposure to daylight can help to lower your risk of developing myopia. Alternatively, cutting down on close-up work can also reduce risk.
-
How does myopia affect children differently than adults?
Myopia often manifests and progresses differently in children compared to adults. In children, myopia typically begins to develop during school age and can progress rapidly during growth phases, particularly during the pre-teen and teenage years. This rapid progression is partly due to the natural growth of the eye, which can elongate and lead to worsening myopia if not monitored and managed effectively.
For children, high myopia increases the risk of developing serious ocular health issues later in life, such as retinal detachment, glaucoma, and early cataract formation. Thus, early detection and proactive treatment are crucial. Interventions might include corrective eyewear (glasses or contact lenses) and newer strategies like orthokeratology (overnight contact lenses that reshape the cornea) or low-dose atropine eye drops, which have been shown to slow the progression of myopia in some children.
Pediatric eye care emphasizes regular eye exams to monitor changes in vision and eye health, ensuring timely adjustments in prescription and the consideration of treatment options that might curb the progression of myopia during the critical growth years.
-
What are the differences between correcting myopia with glasses, contact lenses, and refractive surgery?
Correcting myopia involves several options, each with its own set of advantages and considerations:
Glasses are a simple and non-invasive way to correct myopia. They can also protect the eyes from environmental factors, such as dust and wind. Some people may find glasses uncomfortable, especially when playing sports or during physical activities. Glasses can fog up in certain weather conditions and may not provide peripheral vision as effectively as other options.
Contact lenses conform to the curvature of your eye, providing a wider field of vision and causing fewer visual distortions than glasses. They are suitable for sports and active lifestyles. Contacts require proper hygiene and care to avoid eye infections. They can cause discomfort, especially in dusty or dry environments, and not everyone finds them comfortable to wear.
Refractive surgery can permanently correct the refractive error causing myopia, potentially eliminating the need for glasses or contact lenses. It is typically a quick procedure with a short recovery time. As with any surgery, there are risks involved, including potential complications such as dry eyes, halos, and other visual disturbances. It’s also usually more costly upfront compared to glasses or contacts and may not be suitable for everyone depending on the eye structure and health.
-
What are the latest advancements in myopia treatment?
Recent advancements in myopia treatment primarily focus on methods to slow its progression in children, as early intervention can reduce the severity of myopia as they reach adulthood. Some of the notable advancements include:
- Low-Dose Atropine Eye Drops: These have been increasingly used as a preventive treatment to slow the progression of myopia in children. Atropine, a muscle relaxant, has been found effective at very low concentrations, minimizing side effects while still effectively slowing down myopia progression.
- Orthokeratology (Ortho-K): This involves the use of specially designed, rigid contact lenses that temporarily reshape the cornea. Worn overnight, these lenses flatten the cornea and correct the focal point of images on the retina. This not only provides clear daytime vision without the need for glasses or contact lenses but also has been shown to slow the progression of myopia.
- Multifocal Contact Lenses: These lenses, which have different power zones, are designed to correct nearsightedness and also to affect how light focuses on the periphery of the retina, which is thought to impact myopia progression.
- MiSight 1 Day Contact Lenses: Approved by the FDA, these soft, disposable, multifocal lenses are designed specifically for children and have been clinically proven to significantly slow the progression of myopia when worn regularly.
These treatments represent a shift from merely correcting vision to actively managing the progression of myopia, aiming to improve long-term visual outcomes for individuals with this condition.
