fix your eyes
on what matters most
Keratoconus Treatment in Melbourne & Brevard County , FL
Keratoconus is caused when the cornea begins to develop into a cone-shape. This eye disease is progressive and has no cure. However, there are treatments in place to help manage the disease, including surgeries and cross-linking therapies.
KERATOCONUS Symptoms
If you have keratoconus, you may see signs of the following:
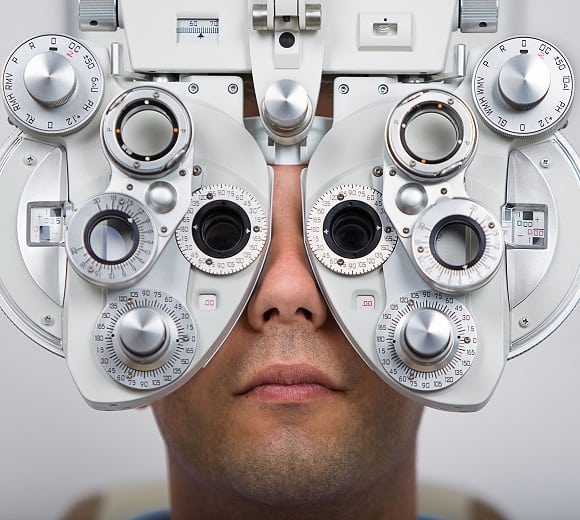
COMPLETE KERATOCONUS TESTING
Diagnosis/ Testing of Keratoconus
Our first-in-class technology suite provides better detection & better outcomes for your vision health.
-
Eye Health Assessment
-
Muscle Function Test
-
Binocular Vision Skills Assessment
-
Eye Pressure Test
-
Color Vision Screening
Eye Health Assessment
This assessment uses an ophthalmoscope to examine different parts of your eye. This is a handheld piece of equipment that the doctor will use to examine your eyes with a light adjusted to the right aperture and filter necessary to see to the back of your eye.
Why We Use This Method:
- This tool allows the doctor to evaluate your pupil responses, optic nerve, retina, cornea, and lens.
- We use this tool to look for signs of eye diseases or retinal vascular diseases.
Muscle Function Test
If you’ve ever had an optometrist ask you to follow an object with only your eyes without moving your head then you’ve completed a muscle function test. The object, commonly a pen or pencil, will be held 40cm from your face while the assessment is completed and generally takes less than 30 seconds to complete. This is performed to check the movement of your eyes in each direction and at specific angles. The doctor will then be able to determine muscle weakness or involuntary eye movement.
Why We Use This Method:
- This checks for uncontrolled eye movement or double vision in patients.
- We’re also able to identify the following potential problem: nystagmus, strabismus, mechanical restrictions due to traumatic injury.
Binocular Vision Skills Assessment
Binocular vision skills assessment aren’t routinely performed on every patient. But if patients complain of indicative symptoms this can be completed to make sure they aren’t suffering from a difficult to detect visual deficit. Failing this assessment could point to you suffering from improper depth perception, poor eye muscle coordination and the inability to change focus from near to far objects.
Why We Use This Method:
- If patients are suffering from the following symptoms we will conduct a binocular vision skills assessment: double vision, headaches, eyestrain, and patients with a traumatic brain injury.
- This assessment identifies the following: oculomotor dysfunctions, accommodative dysfunction, binocular vision dysfunction, strabismus, visual perceptual deficits.
Eye Pressure Test
Your doctor may administer one or more tests to evaluate your intra-ocular pressure. One commonly used test is through the use of a machine, that puffs air into your eye to test IOP call a non-contact tonometry (NCT). The eye bounces the air back to a sensor that reads the pressure automatically. While unpleasant, this test is not painful.
An alternative way to perform this test in the case of a NCT machine being unavailable is through manual testing. Eye drops will be administered and then gentle pressure will be applied to the surface of your eye by the ophthalmologist or using a blue light instrument. This will feel like placing a contact lense in your eye.
The desired range for eye pressure will vary from person to person but your ophthalmologist will determine the correct range for you individually. High intra-ocular pressure could point to glaucoma developing in your eyes which will need to be addressed further by the ophthalmologist.
Why We Use This Method:
- The major purpose behind testing eye pressure is to identify eyes developing glaucoma.
Color Vision Screening
Color vision screening is used to see how you perceive colors. Color blindness doesn’t generally affect everyday life. It is usually tested using a form of the Ishihara but more intensive forms of assessment are available. Extensive exams look into the type and severity of color blindness while color vision screening only shows if there is a color vision problem.
Why We Use This Method:
- Identifying color blindness, especially in children, can explain poor performance or learning frustratio

Eye Health Assessment
This assessment uses an ophthalmoscope to examine different parts of your eye. This is a handheld piece of equipment that the doctor will use to examine your eyes with a light adjusted to the right aperture and filter necessary to see to the back of your eye.
Why We Use This Method:
- This tool allows the doctor to evaluate your pupil responses, optic nerve, retina, cornea, and lens.
- We use this tool to look for signs of eye diseases or retinal vascular diseases.

Muscle Function Test
If you’ve ever had an optometrist ask you to follow an object with only your eyes without moving your head then you’ve completed a muscle function test. The object, commonly a pen or pencil, will be held 40cm from your face while the assessment is completed and generally takes less than 30 seconds to complete. This is performed to check the movement of your eyes in each direction and at specific angles. The doctor will then be able to determine muscle weakness or involuntary eye movement.
Why We Use This Method:
- This checks for uncontrolled eye movement or double vision in patients.
- We’re also able to identify the following potential problem: nystagmus, strabismus, mechanical restrictions due to traumatic injury.
Binocular Vision Skills Assessment
Binocular vision skills assessment aren’t routinely performed on every patient. But if patients complain of indicative symptoms this can be completed to make sure they aren’t suffering from a difficult to detect visual deficit. Failing this assessment could point to you suffering from improper depth perception, poor eye muscle coordination and the inability to change focus from near to far objects.
Why We Use This Method:
- If patients are suffering from the following symptoms we will conduct a binocular vision skills assessment: double vision, headaches, eyestrain, and patients with a traumatic brain injury.
- This assessment identifies the following: oculomotor dysfunctions, accommodative dysfunction, binocular vision dysfunction, strabismus, visual perceptual deficits.

Eye Pressure Test
Your doctor may administer one or more tests to evaluate your intra-ocular pressure. One commonly used test is through the use of a machine, that puffs air into your eye to test IOP call a non-contact tonometry (NCT). The eye bounces the air back to a sensor that reads the pressure automatically. While unpleasant, this test is not painful.
An alternative way to perform this test in the case of a NCT machine being unavailable is through manual testing. Eye drops will be administered and then gentle pressure will be applied to the surface of your eye by the ophthalmologist or using a blue light instrument. This will feel like placing a contact lense in your eye.
The desired range for eye pressure will vary from person to person but your ophthalmologist will determine the correct range for you individually. High intra-ocular pressure could point to glaucoma developing in your eyes which will need to be addressed further by the ophthalmologist.
Why We Use This Method:
- The major purpose behind testing eye pressure is to identify eyes developing glaucoma.
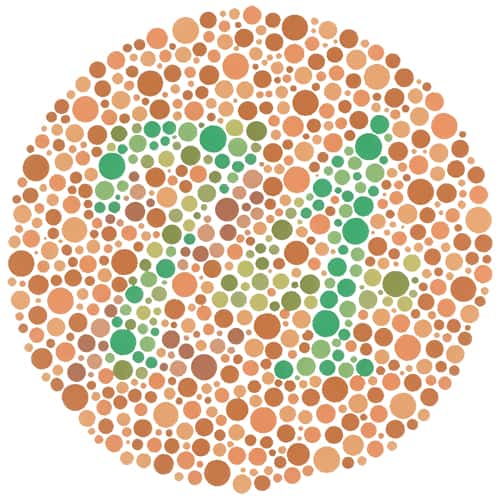
Color Vision Screening
Color vision screening is used to see how you perceive colors. Color blindness doesn’t generally affect everyday life. It is usually tested using a form of the Ishihara but more intensive forms of assessment are available. Extensive exams look into the type and severity of color blindness while color vision screening only shows if there is a color vision problem.
Why We Use This Method:
- Identifying color blindness, especially in children, can explain poor performance or learning frustratio
Treatment Options
Restore your vision & restore your life with the most modern keratoconus treatments available today.
Improved Vision: NO CONTACTS OR GLASSES REQUIRED
If you suffer from keratoconus and no longer benefit from contacts or glasses you may be a good candidate. The design of the stabilizing device was created to help fight the effects of keratoconus from the inside-out by working to flatten the cornea. While it won’t cure keratoconus, placement can prevent the need to have a cornea transplant in the future.


Comfortable Recovery Process
The procedure to implant is minimally-invasive, resulting in less trauma to the cornea and surgery site. This aids in a quicker recovery and smaller chance of astigmatism developing. Distortions and scarring will be minimized as well. With the procedure, you with experience an easy recovery process without effect on your daily comfort.
DESIGNED TO BE PERMANENT BUT CAN BE REMOVED
Can Be Exchanged if Vision Changes
You certainly won’t need to worry about it falling out. Nor will you need to worry about permanence due to removal of tissue. Because they are additive, they can be removed in the future should the need arise. If you find your prescription changing dramatically you can even exchange the them for a new pair that match your new vision needs.

IMPROVED VISION WILL BE THE ONLY INDICATOR IT’S THERE
Once administered, you will not feel them in your eyes. Plus they are no more visible than contact lenses. The comfort and subtlety of this treatment option make them attractive to those suffering from keratoconus. An added bonus is the eliminated maintenance. See clearer without the hassle of upkeep.
NO WORRIES ABOUT FOLLOW-UP TREATMENTS
Permanent Results
Corneal cross-linking isn’t a procedure you’ll need to have performed consistently over the period of your life, it’s a one-time treatment. This out-patient treatment will be over in roughly an hour and then you’ll be on your way to enjoying your heightened vision.


TYPICALLY COMPLETE IN 1 HOUR
Simple Out-Patient Procedure
The procedure is non-invasive and lasts for 60 to 90 minutes in length. This simple out-patient procedure only requires that you have a ride home as you won’t be allowed to drive yourself. The recovery time following cross-linking may vary from individual to individual. But generally, it takes a week to recover.
Laser-Assisted CORNEAL TRANSPLANTATION PROCEDURE
Intralase Enabled Keratoplasty (IEK) is a laser assisted surgery for corneal transplantation. The use of the laser increases the precision of the procedure resulting in more favorable outcomes.


Prevent Keratoconus Progression/ Corneal Transplants
By strengthening the links between the cornea and collagen fibers you can prevent the progression of keratoconus. This is a non-invasive way to handle keratoconus compared to common alternatives like corneal transplants.
OPTIMAL CORNEAL TRANSPLANTATION METHOD
Improved Visual Outcome with Less Astigmatism
With the IEK surgery, ophthalmologists are able to increase visual outcomes that result in less surgery-induced astigmatism. This results in better vision for you now with fewer complications down the road.


REDUCE PAIN, RESTORE VISION & IMPROVE APPEARANCE OF CORNEAS
Intralase Enabled Keratoplasty – Corneal Transplant Surgery
Corneal transplant surgery treats diseases that originate in the cornea by transplanting a cornea from a donor to you. This method of treating keratoconous is shown to be a safe, beneficial alternative to other methods. You can expect a faster recovery time and improved vision after surgery.
QUICKER HEALING THAN ALTERNATIVE PROCEDURES
Fast Healing Time
Within two to three months after surgery, you will be able to see with limited functionality without the use of glasses or contacts. Their vision will strengthen over the following months, achieving 20/40 or better after six to seven months. This is a huge improvement from the alternative surgery which requires a twelve to eighteen month recovery period.


MORE BENEFICIAL THAN STANDARD SURGICAL PRACTICES
Safe and Effective
IEK will result in less astigmatism caused by the surgery and will result in quicker recovery time. This effective and safe procedure has a rare chance of transplant failure and transplants are checked intensively for suitability to your eye.
FAQ
-
Who is at risk of developing keratoconus?
If you tend to rub your eye vigorously or have a family history of keratoconus, you may have a heightened risk of developing keratoconus. The presence of other diseases can also raise your risks. These include:
- Asthma
- Hay Fever
- Ehlers-Danlos syndrome
- Down syndrome
- Retinitis pigmentosa
-
How can I prevent keratoconus from worsening?
Keratoconus is a lifelong disease of the eye. Once diagnosed, your doctor will develop a treatment plan. Your best option for preventing further progression of keratoconus is to follow the recommended treatment plan and regularly receive eye exams.
-
What happens if keratoconus is left untreated?
If left untreated, keratoconus can result in partial or complete loss of vision. This disease can be monitored and progression can be halted by following a treatment plan, however, action will need to be consistently taken throughout your life to prevent the effects of untreated keratoconus from setting in.
-
Is keratoconus hereditary
Research on keratoconus is still being conducted to understand exactly what causes the disease to take hold. Keratoconus is partially hereditary but also influenced by outside behavioral and environmental factors. If you have a family history of keratoconus the genetic factors are present which will increase your risk for developing the disease. However, unless you encounter certain behavioral and environmental factors in your life the disease may not develop.
-
Is keratoconus permanent?
Yes. Presently, there are no known cures for keratoconus. If you have been diagnosed with keratoconus you will need to prepare for a lifelong treatment plan to control the progression of the disease.
-
What is the benefit of corneal cross-linking?
Corneal cross-linking adds stability to the eye by building links to collagen that holds the cornea in place. This can prevent. This procedure is minimally-invasive which is an added benefit given alternative treatments for keratoconus include cornea transplant which is a highly invasive surgery.
-
How long will pain last after corneal cross-linking?
Your eyes will be sensitive and painful for three to five days following the procedure. Your pain levels may vary from other patients.
-
How long does it take to recover from corneal cross-linking?
It can take up to a week to fully recover from corneal cross-linking. Be aware, recovery time varies and you may experience a recovery period lasting longer than seven days.
-
How long does corneal transplant surgery take?
Corneal transplant surgery takes between 30 minutes and one hour. This excludes time needed to prep and post-surgery procedures
-
What to expect after corneal transplant surgery?
After the surgery, you will need to have transportation home. Your eyes will likely have sutures but these will be unnoticeable.
You should avoid activities that could potentially effect your eye. This includes activities such as contact sports. Your doctor will provide you with more information on precautions during your recovery process.
-
How long does it take to recover from corneal transplant surgery?
After corneal transplant surgery, it typically takes about one to two weeks to resume normal activity. Actual recovery time will depend on if you had a partial or full-thickness transplant. Your doctor will be able to give you a more specific timeline to full recovery.
-
What causes keratoconus?
Keratoconus is a progressive eye condition in which the normally round cornea thins and begins to bulge into a cone-like shape. This deformation deflects light as it enters the eye on its way to the light-sensitive retina, causing distorted vision. The exact cause of keratoconus is not well understood, but it is believed to be a combination of genetic predisposition and environmental factors. Some studies suggest that excessive eye rubbing, a history of poorly fitted contact lenses, and chronic eye irritation may contribute to its development. Additionally, it often appears in the teenage years or early twenties and can be associated with certain allergic conditions like asthma and eczema, which indicate a possible link to an allergic or atopic background.
-
When should you see a doctor about keratoconus?
It’s important to consult an eye care professional if you notice any changes in your vision, particularly if you experience sudden vision distortion or blurring, increased light sensitivity, or if your eyeglass prescriptions change frequently, which are common signs of keratoconus. Early diagnosis and treatment of keratoconus are crucial for slowing its progression and improving vision. Regular eye exams are recommended, especially for teenagers and young adults, as keratoconus typically begins at puberty and progresses into the mid-thirties.
-
What other eye conditions are associated with keratoconus?
Keratoconus can be associated with several other eye conditions, including:
- Vernal keratoconjunctivitis: A seasonal allergic condition that affects the surface of the eye.
- Retinitis pigmentosa: A group of rare, genetic disorders that involve a breakdown and loss of cells in the retina.
- Down syndrome: Individuals with Down syndrome are significantly more likely to develop keratoconus.
- Ehlers-Danlos syndrome: A group of disorders that affect connective tissues, including those in the eyes.
- Leber congenital amaurosis: A genetic disorder that primarily affects the retina and can be associated with keratoconus due to the overall fragility in the eye structure.
Understanding these associations is important for comprehensive care and may influence the management strategies for keratoconus.
-
What lifestyle adjustments should someone with keratoconus consider to manage their condition?
Managing keratoconus involves both medical treatments and lifestyle adjustments to help stabilize the condition and maintain the best possible vision quality. Here are some key lifestyle adjustments that individuals with keratoconus might consider:
- Avoid Eye Rubbing: One of the most crucial adjustments is to avoid rubbing the eyes. Eye rubbing can exacerbate the thinning of the cornea, accelerating the progression of keratoconus. If eye itching is a problem, it’s important to consult with an eye care professional about appropriate treatments for allergies or irritations that might cause rubbing.
- Use Protective Eyewear: For those involved in sports or occupations that pose a risk of eye injury, wearing protective eyewear is essential. Injuries can worsen the condition or trigger progression in a previously stable eye.
- Manage Allergies Effectively: Since allergies can trigger eye rubbing, managing them with appropriate medications can be a key part of keratoconus management. Over the counter or prescription allergy medications may be recommended to control symptoms.
- Follow Regular Eye Examination Schedules: Regular follow-ups with an eye care provider are vital. These visits allow for monitoring of the condition’s progression and adjustments in treatment as needed. Early detection of changes can lead to earlier intervention, which may help slow the progression of the disease.
- Adopt a Healthy Lifestyle: General health impacts eye health, so maintaining a balanced diet, staying hydrated, and getting enough sleep are all beneficial for overall eye health.
- UV Protection: Wearing sunglasses that offer UV protection is important to protect the eyes from harmful ultraviolet rays, which can contribute to eye strain and damage.
Implementing these lifestyle changes can play an important role in managing keratoconus, complementing medical treatments such as corneal cross-linking or specialized contact lenses designed to help maintain vision quality and eye health.
